Postoperative pain management any practice can afford
Effective pain management in postoperative patients is possible no matter the size or focus of the veterinary practice. Consider the wide range of economical drugs available to help reduce pet suffering and pain.
In human medicine, pain is considered the fifth vital sign, ranking as important as pulse, respiration, temperature, and blood pressure. Pain also continues to gain attention in veterinary medicine as an important vital sign. Pain can have many negative side effects in our patients, including tachycardia, hypertension, immunosuppression, delayed wound healing, exhaustion, and inappetence.1
However, most technicians and veterinarians lack current knowledge of common analgesics, local anesthetic agents, and adjunctive analgesics with regard to their pharmacology, duration of action, and cost. Educating veterinarians and technicians with regard to the affordability of these drugs and their actions should increase multimodal analgesia in single-doctor and multidoctor practices, resulting in better pain management for postoperative patients.
Assessing pain
Unfortunately, our patients cannot tell us when they are experiencing pain, so we must learn to watch and listen to our patients. Patients experiencing pain will exhibit many behavioral changes, including guarding or biting of the surgical site, aggression, or a frequent changing of positions. Some patients will assume a prayer-like position, especially after postoperative abdominal or thoracic surgery.
Many pain scoring techniques are available in veterinary medicine, and they can be helpful tools when implemented correctly. But ultimately, it is the technician's responsibility to observe changes in both the patient's behavior and vital signs and to notify the veterinarian of any clinical signs of pain. It is also our duty as technicians and veterinarians to educate owners about these signs so their pets can comfortably convalesce at home.
Understanding pain pathways
The pain pathway consists of four processes: transduction, transmission, modulation, and perception.
1. Transduction is the site at which a painful (noxious) stimulus occurs and is converted into an electrical signal that will be transmitted to the central nervous system (CNS) through afferent nerves (nerves that carry electrical signals toward the CNS).
2. The transmission portion of the pathway involves peripheral nerves that send the noxious stimulus to the dorsal horn of the spinal cord, then through the spinal cord, and finally to the brain. These peripheral nerves contain both afferent and efferent (nerves that carry the electrical signal away from the CNS) nerves.
3. Modulation alters the noxious signal; i.e., the signal is either amplified or suppressed. Modulation occurs in the spinal cord as well as the brain.
4. Finally, during perception, the brain deciphers the information that it has received and interprets that information as pain.
Figure 1 shows the different pain pathways as well as the analgesics, nonsteroidal anti-inflammatory drugs (NSAIDs), and local anesthetics that can be administered to treat pain at different points in the pathway. (Note: Several other drugs that affect the pain pathway are beyond the scope of this article. These drugs can be located in current anesthesia and pain management textbooks.)
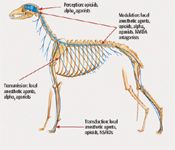
Figure 1: Diagram of the canine nervous system. (Dorling Kindersley/Thinkstock)
Disruption along the pathway occurs when analgesics, NSAIDs, and local anesthetic agents are used. Multimodal pain management targets several of these pathways at the same time, resulting in better analgesia. NSAIDs are an important part of multimodal analgesia, and many articles have been written on their positive contributions. They should be considered when developing a postoperative multimodal pain management strategy. However, this article will limit discussion to the economical cost of different opioids, local anesthetic agents, and adjunctive analgesics and how these drugs contribute to better analgesia than what is currently being used in many small and large veterinary practices.
Opioids
Opioids act at three points along the pain pathway to provide analgesia. However, not all opioids act in a similar manner. Opioids are divided into three categories: full mu agonists, partial mu agonists, and agonist-antagonists.
Full mu agonist opioids, such as morphine, methadone, and hydromorphone (Figure 2), give the best pain relief because they fully attach to the mu receptor site (the primary opioid receptor). One drawback: Full mu opioids can cause patients to vomit. Methadone is more expensive than many other full mu opioids, but it is gaining in popularity because it rarely causes vomiting in dogs, and cats experience euphoria.2 All full mu opioids used in veterinary medicine are classified as Schedule 2 narcotics requiring additional Drug Enforcement Agency paperwork. However, this is not a valid reason not to carry at least one full mu opioid. Our duty as both veterinarians and technicians is to provide as much pain relief as possible to our patients.

Figure 2: Methadone (on the left) is the most expensive of the opioids shown, but it is gaining popularity because it rarely causes vomiting in dogs, and cats experience euphoria.2
Partial mu agonists, such as buprenorphine, do not attach fully to the mu receptor and give less pain relief them full mu agonists. They take longer to take effect—20 to 30 minutes when given intravenously, 45 minutes when given intramuscularly, and up to one hour when given orally. Subcutaneous administration is discouraged, as recent studies show that this route is not very effective.3 However, buprenorphine is commonly used in cats to treat postoperative pain and is given orally. Current doses range from 0.01 to 0.04 mg/kg every eight to 12 hours.4 Buprenorphine has a ceiling effect, so increasing the dose will not cause any further pain relief but may increase the time between doses.4 Buprenorphine can become expensive if large volumes are used, but it remains an economical choice for small patients.
Opioid agonist-antagonists, such as butorphanol, provide little pain relief because they block the mu receptor site and will reverse full mu opioids if given together or within a few hours of each other. Agonist-antagonists are best used for procedures requiring sedation only with little or no analgesia.
Morphine is an economical opioid (Table 1) when compared with several different competing opioids. It is a full mu agonist, so patients receive better analgesia with morphine than with buprenorphine. Hydromorphone is another inexpensive alternative, but its lower concentration and shorter duration of action (two hours) can make it more expensive to administer than morphine. Morphine's duration of action lasts about four hours, but it can be given as frequently as every two hours or as infrequently as every six hours.
Table 1: Cost of common pain management drugs in dogs and cats*
Patients need to be assessed postoperatively to determine a dosing schedule that best suits their analgesic needs. Morphine rarely causes vomiting beyond the first dose and is most effective if given intramuscularly. Morphine can be given intravenously, but use caution as it is more likely to cause a histamine reaction when administered by this route. Morphine can be safely used in cats. Incidents of cats becoming extremely dysphoric after receiving morphine as an analgesic have been alleviated in recent years because it has been recognized that cats have a low level of the primary metabolic pathway for morphine.5 Current morphine doses in cats range from 0.05 to 0.1 mg/kg, which are about 10 times less than doses in dogs.5
Local anesthetic agents
Local anesthetic agents are an extremely inexpensive solution for alleviating pain at the source (Table 1). Agents such as lidocaine and bupivacaine work directly at the site of transduction and can stop or minimize pain signals from moving up the pain pathway.
Lidocaine is a relatively short-acting local anesthetic agent (about 30 to 60 minutes) with a rapid onset. Bupivacaine has a slower onset (10 to 20 minutes) but is longer-acting. Bupivacaine without epinephrine usually has a two- to four-hour duration of action, whereas bupivacaine with epinephrine can have a duration of four to six hours. Bupivacaine with epinephrine increases the duration of the block by causing vasoconstriction of the surrounding vessels, allowing the bupivacaine to reside in the affected area longer. Bupivacaine with epinephrine should not be used on tissues that might have a compromised blood flow because the epinephrine will cause vasoconstriction of the surrounding blood vessels, resulting in decreased blood flow to an already compromised tissue bed.
Incisional blocks as well as selective nerve blocks for feline onychectomies or tendonectomies are simple and easy to perform and greatly add to a multimodal pain management protocol. Incisional blocks can be performed either before subcutaneous closure (i.e., after the body wall has been closed) or after all layers of the incision have been closed. Bupivacaine is injected along the side of the incision at a dose of 1 to 2 mg/kg with a 25- or 22-ga needle.
Selective nerve blocks are another useful tool in multimodal pain management, with pictures and diagrams being found in many current anesthetic and pain management textbooks.6
Diffusion wound catheters (MILA International) are another option if wounds are large and traumatic. The catheters use inexpensive local anesthetic agents and are economical to purchase or make.7 These catheters dramatically reduce postoperative pain associated with limb amputations, thoracotomies, mammary chain excisions, or large mass removals and will aid in reducing the amount of opioids administered postoperatively.
The catheter works much like a soaker hose for your garden. It contains many tiny holes down its length and is placed in the deepest area of the surgical site. Once wound closure is complete, an injection cap is placed on the open end of the catheter and bupivacaine infusion can begin. A dose of 0.5 mg/kg (cats) or 2 mg/kg (dogs) is injected every six to eight hours.7 A concentration of 0.25 percent bupivacaine is ideal for infusing diffusion wound catheters in cats or small dogs, whereas 0.5 percent bupivacaine works well in larger dogs.7
The priming volume will be noted on the package of purchased catheters, so the first dose in a small patient may require two doses—one to load the catheter and the other to infuse the site. Sterility should be strictly enforced. Wipe injection ports with alcohol before infusing bupivacaine into the catheter. Diffusion wound catheters should be left in place for one to three days—the most painful period of postoperative recovery (Figure 3). Patients can be sent home with the catheters in place as long as clients understand the importance of maintaining sterility when injecting bupivacaine into the catheter.

Figure 3: A cat after an amputation with a diffusion wound catheter. The catheter was maintained three days after surgery along with additional analgesics. (Photo courtesy of Dr. Karen Kaplan)
Adjunctive analgesics
Drugs that provide analgesic properties for painful conditions but that were originally used for other conditions are adjunctive analgesics. Tramadol and gabapentin are the most frequently used adjunctive analgesics. These drugs are inexpensive (Table 1) and can relieve both chronic and postoperative pain.
Tramadol has been widely used in veterinary medicine for the last several years. It is a synthetic, nonscheduled analgesic that is a weak mu receptor agonist. It has been used to manage postoperative pain in dogs and is not used in cats. However, the veterinary dose and duration far exceed the human recommended dose. Recent studies in dogs have shown that the drug has a short half-life of about two hours, requiring dosing at least every six hours to maintain adequate pain control.8 Subtherapeutic doses for patients can occur if owners are unable to follow this schedule, resulting in breakthrough pain. This may lead to poorly managed pain, causing patients to suffer from hyperalgesia (excessive pain response from a noxious stimulus) or allodynia (pain response from a stimulus that does not usually cause pain). The International Veterinary Academy of Pain Management (IVAPM) recommends doses that are greater than those administered by most veterinarians—5 to 15 mg/kg four times daily in postoperative canine patients.9
Gabapentin is another adjunctive analgesic originally developed to control seizures in people. However, its primary purpose now is to control chronic pain in both human and veterinary patients. Gabapentin has been used to control pain in patients suffering from osteoarthritis and cancer. However, it is useful for postoperative pain associated with limb amputations, intervertebral disk surgery, fractures, or any other exceedingly painful surgical procedure. The drug is excreted by the kidneys, and starting dosages in dogs range from 5 to 15 mg/kg given two to three times a day. However, doses of 30 to 40 mg/kg two to three times daily are not unheard of in dogs with chronic pain.6 Gabapentin can cause patients to become sleepy when initial treatment is started or when the dosage is increased. It is recommended that dosing start initially at a rate of once a day given in the evening for the first several days until the patient adjusts to the drug or when an increase in the drug dosage occurs. Gabapentin can be used in cats as well. The human oral solution of gabapentin should not be used because it contains xylitol. Veterinary compounding pharmacies make non-xylitol-containing gabapentin. The oral solution is great for small dogs as well as cats. Doses in cats start at 25 to 50 mg once daily for the average feline patient.
Conclusion
Great pain management is no longer out of reach for the small veterinary practice. With the wide range of economical drugs available to all veterinary practices, no veterinarian, technician, or pet owner has to witness a pet suffering in pain. It is ultimately up to the practice owner or owners to make the vital and necessary changes to improve pain management in their hospital or clinic by familiarizing team members—both veterinarians and veterinary technicians with many of the old and new drugs available today to treat pain. The key is developing a multimodal approach that uses full mu opioids, local anesthetic agents, NSAIDs, and adjunctive analgesics so that every patient in the veterinary hospital receives adequate analgesia.
Susan Burns, BS, RVT, VTS (Anesthesia), is a technician at East Bay Veterinary Specialists in Walnut Creek, Calif. She has a private veterinary anesthetic consulting business and speaks on the topics of anesthesia and pain management.
References
1. Lockhead K. Pain Assessment. In: Bryant S, ed. Anesthesia for veterinary technicians. 1st ed. Ames, Iowa: Wiley-Blackwell, 2010;334-335
2. Papich M. Saunders handbook of veterinary drugs: Small and large animals, 3rd ed. St. Louis, Mo. Elsevier Saunders, 2011:483-485
3. Giordano T, Steagall P, Ferreira T, et al. Postoperative analgesic effects of intravenous, intramuscular, subcutaneous or oral transmucosal buprenorphine administered to cats undergoing ovariohysterectomy. Vet Anaesth Analg 2010;37(4):357-366.
4. Veterinary Anesthetic Support Group. http://www.VASG.org. Accessed: October 26, 2012.
5. Lamont L, Mathews K. Opioids, nonsteriodial anti-inflammatories, and analgesic adjuncts. In: Tranquilli WJ, Thurmon JC, Grimm KA, eds. Lumb & Jones' veterinary anesthesia and analgesia. 4th ed. Ames, Iowa: Wiley-Blackwell, 2007;245-246.
6. Spelts K, Gaynor J. Pain management strategies. In: Bryant S, ed. Anesthesia for veterinary technicians. 1st ed. Ames, Iowa: Wiley-Blackwell, 2010;350-352.
7. Hardie E, Lukasik V. Orthopedic patients. In: Tranquilli WJ, Thurmon JC, Grimm KA, eds. Lumb & Jones' veterinary anesthesia and analgesia. 4th ed. Ames, Iowa: Wiley-Blackwell, 2007;1014.
8. Kukanich B, Papich MG. Pharmacokinetics of tramadol and the metabolite O-desmethyltramadol in dogs. J Vet Pharmacol Ther 2004;27(4):239-246.
9. Downing R. IVAPM Daily Digest, June 12, 2012.