Dermatology: 6 crucial skills for veterinary technicians
Whether cleaning the ears of floppy-eared dogs or setting up the exam room, technicians are an important part of dermatology case management.
Examining the skin is relatively straightforward because the diseased organ can be seen and palpated by the veterinarian—and by technicians and owners. Technicians can—and should—play an integral role in skin disease cases. They can help save the doctor time as well as increase client compliance.

Each clinic has different rules regarding what a technician can and can't do. However, some general areas where you may be valuable include: setting up the examination room for a dermatology case, obtaining skin samples, analyzing samples and recording results, and educating clients about how to properly perform certain diagnostic tests and treatments (Table 1). Many technicians also will perform the initial history and examine ears.
1. Setting the room
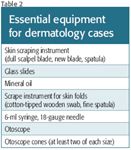
Any time patients present with skin or ear diseases, certain equipment will be needed in the examination room (Table 2). It is your job to make sure the room is adequately equipped to save the veterinarian's time.
The necessity for multiple otoscope cones, so that each ear can be examined with a clean cone, is often neglected. Various sizes of otoscope cones are also needed to examine the ears of different breeds of dogs and cats. Cones need to be properly cleaned before use. To do that, scrub the cone, place in an effective disinfectant for at least 10 minutes, rinse, and then let it dry.
Another common setback is poorly charged handheld otoscopes. Otoscopes must have a strong light and power source and at least 10x magnification that allows for focusing within the normal length of the ear canal. If battery-charged lights are used, make sure they are fully charged. When the batteries no longer give a bright light or do not hold a charge for long, they should be changed. In addition, every clinic should have at least one plug-in otoscope that is not dependent on fresh, fully charged batteries.
Many practitioners use diagnostic otoscope heads. However, surgical otoscope heads allow more manipulation and angulation and are easier to use with cleaning and therapeutic procedures that require passing instruments or tubes into the ear canal with concurrent visualization. Know what is preferred in your practice, or by each veterinarian, and make sure that exam rooms are appropriately equipped.
2. Routine skin sampling
Skin samples are almost always needed, and in many clinics, technicians play a large role in this task. The first step is to determine what tests are needed and what is being tested for. The veterinarian will make this decision, generally after reviewing the history and examining the patient. Once that decision is made, then the technique for acquiring the sample will be determined. Then you—or the veterinarian, depending on your clinic's protocol—will acquire the necessary sample.
After the sample is obtained, it may require processing or preparation. In most practices, a technician performs this task. The sample will need to be evaluated with a microscope. Even if you are not performing the microscopic evaluation, properly taking and processing samples and placing them by the microscope saves time during an examination.
3. Skin scraping
Skin scraping—one of the most frequently performed tests in veterinary dermatology—is recommended anytime the differential diagnosis list includes microscopic ectoparasitic diseases. Skin scraping is most commonly used to verify or rule out demodectic mange. It is also commonly performed to help diagnose sarcoptic mange (although it does not effectively rule out sarcoptic mange), Cheyletiella species infestations, and other ectoparasitic diseases.
The collected material is placed on a microscope slide and mixed with oil. It is preferable to use a cover slip, but many practitioners do not. The cover slip puts the material in a flat plane, which facilitates examination and decreases the chance of getting oil on the lens. The key to a complete examination is that all the collected material be examined with a consistent, orderly approach. When looking for mites that are relatively large and clear, it is best to lower the condenser source, which results in better visualization. Since mites are relatively large, the material can be examined at low power (4x or 10x).
Use a Z pattern to ensure all material is examined. Start at one corner and move the slide in one direction to the end of the sample. Next, move to the adjacent field with just slight overlap of the previous field. Then move the slide and examine the material back on the initial slide. If you see a suspicious object at low power, you can change to a higher power to better identify it. Be very careful to not let the lens get into the oil. There is no need to use an oil immersion.
DEMODECTIC MITES
Skin scraping seems to be a straightforward laboratory procedure. However, specialists see many demodicosis case referrals in which skin scrapings were not performed, or false negative skin scraping findings led to misdiagnosis.
Generally, multiple scrapings from new lesions should be obtained. For Demodex species, small areas are all that need to be scraped, and the key is to scrape deep enough. The affected skin can be squeezed to extrude the mites from the hair follicles. It is helpful to apply a drop of mineral oil to the site being scraped or to the scalpel blade or spatula to facilitate the adherence of material to the blade. Additional material is obtained by scraping the skin deeply until capillary bleeding is produced. The hair plucking technique can be used in areas where skin scrapings may be more difficult (periocular, interdigital). With this technique, hairs are gently plucked and are examined in mineral oil on a glass slide, as you would with a skin scraping. Often, mites can be identified on the hair bulb. With either technique, it is important to note the approximate number of mites you see and the ratio of live to dead mites. You should also identify the relative number of each stage—adult, larvae, and egg—and enter this into the patient's record. Some clinics use a form for each scraping.
SCABIES MITES
Canine sarcoptic mites reside within the superficial epidermis. However, because small numbers of mites are usually present, they are difficult to find. In contrast to scrapings for Demodex species, scrapings for suspected scabies are superficial and should cover large areas. Multiple superficial scrapings are indicated, with emphasis on the pinnal margins and elbows. The more scrapings performed, the more likely a diagnosis. However, even with numerous scrapings, scabies cannot be ruled out because of negative results. Nevertheless, skin scrapings should be performed on any chronically, poorly responsive pruritic dog. Unlike in demodicosis cases, when examining the collected material, numbers are irrelevant. So once a mite, eggs, larvae, or even mite feces are seen, the diagnosis is confirmed and the rest of the material does not need to be examined.
4. Examining ears
A veterinarian usually performs an otoscopic examination, especially for new cases. A technician may also perform an examination during an ear cleaning to see if the cleaning was effective.
A proper otoscopic examination allows as complete visualization as possible with minimal pain or trauma. Many dogs or cats resist and make it impossible to complete an examination if the technique is not optimal. Animals with inflamed, painful ears may also increase the difficulty of an examination.
Examinations are usually best done on a table to allow for appropriate scope orientation. Large dogs may be examined on the floor if you are kneeling and the dog's head is held high enough to allow the otoscope to move into a horizontal position. Occasionally, it is easier to examine an ear if the dog lays in lateral recumbence on the table.
The muzzle should be directed slightly toward the thoracic inlet. The natural tendency is for the head to be tilted as the examination starts, but that redirects the cone tip, resulting in pain. The pinna should be pulled up and out from the base of the skull, which helps to straighten the ear canal and minimize the blocking of the lumen by the auricular projection that is present near the junction of the vertical and horizontal canal.
Pass the cone tip down the lumen of the ear canal while you visualize the canal through the otoscope cone. Attempting to insert the cone without visualization is a sure way to hit the canal epithelium, which can be painful even in a normal ear. Then move the cone slowly into the vertical canal, visualizing as you go. Rotate the otoscope handle downward, so the cone approaches a horizontal position. The movement is best accomplished when the ear is also pulled up and out over the cone tip so that the two processes happen simultaneously. Proper placement at the junction often allows visualization into the horizontal canal and, if necessary, advancement into the horizontal canal. Deep penetration into the horizontal canal is done only to visualize the tympanum. Note any redness, exudate, foreign objects, mites, polyps, or tumors.
5. Diet trials
Diet trials are often part of the work up of itchy dogs. Many times clients spend a lot of time and money performing diet trials and become frustrated when they find out they did not perform a trial correctly. Your job is to emphasize to owners that it is crucial that nothing be ingested or swallowed by a dog on a hypoallergenic diet trial except the food the veterinarian recommended. Anything else, whether given intentionally or found by the dog, can ruin the trial. Always explain this key point to owners.
6. Cleaning ears
Keeping ears clean is the most important aspect of treating proliferative otitis. To accomplish this, clients must be able to perform cleanings at home. Otherwise, frequent followup visits for cleaning will be required.
Cleaning is helpful for several reasons. Debris and microbes are removed, thus decreasing overgrowth and the environment favorable to overgrowth. Inflammatory mediators are also removed, and folds are temporarily opened. A clean ear is more likely achieved with topical medication. Pressure from debris is at least temporarily removed from the deep ear canal and tympanic membrane, if it is still present. In atopic dogs, allergens present on the skin surface or trapped within the cerumen and debris on the pinna and in the ear canal are also removed or at least decreased. In severely inflamed, painful ears, home cleaning should be delayed, because many dogs will not tolerate it until after the inflammation and pain have resolved. Thus, home cleaning is usually recommended following the initial therapy.
There are two main ways for clients to clean ears at home: using an ear wash or by bulb syringing. Using an ear wash is the most common method. With this technique, the client places a mild cleanser in the ear until the canal has been filled to the external orifice and applies the cleanser to the external orifice and concave pinna. This technique tends to be a little messy and should be done outside, in a bathroom, or even in a shower stall.
There are two important aspects to this technique. First, since the cleanser may not be rinsed out, it must be nonirritating and safe to leave in an ear. Numerous veterinary otic cleansers are available. Generally, it is best for the cleanser to be alcohol-free and gentle, and to have some disinfectant activity. Second, in dogs with significant horizontal canal buildup, adequate massage of the auricular and annular cartilage is necessary. To effectively massage the annular cartilage, the client must be educated about the location and need for deep digital palpation. Following several minutes of massage, the animal is allowed to shake the material out, and the pet owner wipes the external orifice and concave pinna clean with tissue or cotton balls. Do not allow excessive use of cotton-tipped applicators down the ear canal, as these commonly push debris deeper. In general, the ear wash technique is not as effective as bulb syringing because of its inability to effectively reach the last portion of the horizontal ear canal, which is contained within the bony external acoustic meatus.
Bulb syringing is generally more effective in cleaning the horizontal canal and gets the ear canal cleaner than the rinse technique does. However, it is messier and more labor intensive and requires adequately trained clients and patients that tolerate the procedure. This technique is usually performed only after it has been determined that the ear wash technique is not getting the ears sufficiently clean. Furthermore, the tympanum should be intact if cerumenolytics are going to be used, because the client may not be able to adequately rinse away all residual drugs and, thus, repetitive application could be dangerous. When the tympanum is not intact, the same mild cleansers used for home ear rinsing are used with the bulb syringe.
Clients are best taught how to use the bulb syringe by practicing with air and learning how hard and fast they can squeeze without hearing the air come out of the syringe. Only lukewarm or body temperature fluids should be used for flushing. The nipple of the bulb syringe should be placed loosely in the external orifice of the ear canal so that once the flushing begins, the flush solution can be seen exiting the ear canal. Allowing adequate back flow helps prevent excessive pressure from building up against the tympanum. Flushing is continued with fresh solution until no debris is seen coming from the ear canal. Clients should not use the bulb syringe to aspirate fluid out of the ear, since the syringe may become contaminated with pathogenic organisms. After the ear is flushed with a bulb syringe, a cleanser disinfectant or disinfectant dryer solution is administered to help dry the ear canal and remove residual rinse water.
Final thought
Dermatology is an area in which you can play a substantial role. Performing the tasks and perfecting the techniques described here will expand your value to the practice and result in better case management.
Dr. Craig Griffin is a past president of the American College of Veterinary Dermatology (ACVD) and the founder and co-owner of San Diego-based Animal Dermatology Clinics.