Anesthetic monitoring savvy
Understanding and interpreting data from a multi-parameter monitor is paramount to a successful anesthetic experience in veterinary practice. Consider this advice to understand these vital values and explore what to do when you encounter abnormalities.
We have been taught that anesthesia is 99 percent boredom and 1 percent panic. But what can you do when you find yourself and your patient in that 1 percent? Monitoring an anesthetized patient's vital signs has been made easier in recent years by the affordability of multi-parameter monitors in the small-animal hospital setting. However, many technicians lack either the knowledge or the training to correct abnormalities during the anesthetic period.
Many times the cause of an abnormality can be traced back to the anesthetic protocol, the surgical procedure, or the patient's medical condition at the time of surgery. However, sometimes the abnormalities can be the related to the anesthetic equipment. Since anesthetic monitoring is one of the primary functions that a veterinary technician performs, it is vital that he or she understands how to troubleshoot potential patient- and anesthetic-equipment-related abnormalities.
ECG and cardiac arrhythmias
An electrocardiogram (ECG) is the record of the electrical impulse as it travels through the heart. The electrical impulse of the myocardium arises in the sinoatrial (SA) node located in the right atrium. The sympathetic nervous system (SNS) and parasympathetic nervous system (PNS) innervate the SA node and can either speed up (SNS stimulation) or slow down (PNS stimulation) the heart rate. The atria contract, forming the P wave of the ECG, after which the electrical stimulation is received by the atrioventricular (AV) node. The AV node receives the electrical stimulation and sends it down the septal wall of the ventricles (Q wave) into the base of the ventricles (R wave) and, finally, to the outside of the ventricle walls (S wave), forming the QRS complex on the ECG. The T wave is formed when the heart relaxes and readies itself for another contraction.
Arrhythmias are the most common abnormality on an ECG and should be treated according to the cause of each arrhythmia. The four most common cardiac arrhythmias seen during anesthesia are sinus tachycardia, sinus bradycardia, AV block, and ventricular premature contractions.
• Sinus tachycardia is a regular sinus rhythm at an excessive rate, generally defined as a heart rate greater than 200 beats/min in cats and greater than 160 beats/min in dogs. When the heart rate is too fast, the ventricles do not have time to adequately refill, so stroke volume declines and hypotension occurs. Tachycardia also increases myocardial work and oxygen consumption. Diagnosing the cause of the tachycardia during anesthesia is paramount in determining the correct course of action. Some causes of tachycardia in anesthetized patients include drug administration (e.g., anticholinergics and sympathomimetics), inadequate anesthetic depth, short-term hypercapnia, anemia, hypovolemia, and undiagnosed hyperthyroidism. If the sinus tachycardia is due to hypovolemia, then determining the degree of loss and whether it is ongoing is crucial. If the volume loss is not great, increasing crystalloid fluid rates may solve the problem. If the volume loss is large or ongoing, then adding an artificial colloid, such as hetastarch, or natural colloids, such as whole blood or packed red blood cells, may be needed. Surgical stimulation can also cause tachycardia. Assess anesthetic depth regularly and adjust vaporizer settings accordingly or add a continuous-rate infusion of an opioid if the stimulation is pain-related.
• Sinus bradycardia refers to a regular sinus rhythm at a decreased rate, generally defined during anesthesia as a heart rate less than 100 beats/min in cats and less than 60 beats/min in dogs. Smaller and giant breed dogs may vary from these norms. The causes of sinus bradycardia in an anesthetized patient include excessive anesthetic depth, administration of drugs such as opioids and alpha2 agonists, vagal reflex (intubation, oculocardiac reflex), visceral manipulation during surgery, and hypothermia. Bradycardia is common in brachycephalic breeds because of excessive vagal tone. If the bradycardia is caused by increases in vagal tone or opioid use, administering an anticholinergic, such as glycopyrrolate, will usually resolve the problem. Treating alpha2-agonist-induced bradycardia with an anticholinergic is no longer considered a wise choice. Alpha2 agonists cause a "reflective bradycardia"—the bradycardia is caused by peripheral vasoconstriction, so the heart rate decreases because the diameter of the blood vessel has been constricted. Giving an anticholinergic in this case can increase myocardial work, oxygen consumption, and the likelihood of an arrhythmia occurring.1 Partial or total reversal of the alpha2 agonist should be considered if the bradycardia is severe.
• AV block occurs when there is a conduction interruption between the SA and AV nodes (i.e., the electrical impulse does not reach the AV node). There are three general types of AV block. A first-degree AV block occurs when there is a prolonged interval between the P and R wave and is an ECG finding only. Usually no intervention is required unless second and third degree heart block develops. A second-degree AV block (Figure 1) is more common and has no QRS wave associated with the P wave. Administering an anticholinergic intravenously, such as glycopyrrolate, is a common treatment. Third-degree AV block is a complete block of the electical impulse to the AV node. The ventricles depolarize and contract independently, creating an "escape beat" on the ECG tracing. The escape beat tracing is similar to an ECG tracing of a ventricular premature contraction. Third-degree AV block is characterized on an ECG by P waves with no QRS complexes. Any ventricular antiarrhythmic drug therapy including lidocaine and anticholinergics is contraindicated in cases of third-degree AV block. Pacemaker implantation is usually the treatment for this type of block.
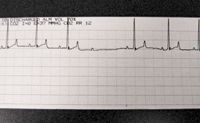
1. An ECG tracing of second-degree AV block. Note the P wave with no QRS associated with it.
• Ventricular premature contractions (VPCs) are ventricular contractions that originate in the ventricular tissue. No pulse is perceived because little or no blood is contained within the ventricle, but a heartbeat will be heard. Some of the most common causes of VPCs during anesthesia are hypoxia, gastric dilatation-volvulus, splenectomies, cardiac trauma, and excitement or fear during induction. If the VPCs are associated with hypoxia, then an increase in oxygen flow should be initiated. This is easily accomplished by decreasing the vaporizer setting. The amount of gas coming from the fresh gas outlet is a combination of oxygen and inhalant. For example, if the vaporizer is set to deliver 2 percent sevoflurane at a 1 L/min flow, then the gas mixture coming from the fresh gas outlet is 0.98 L of oxygen and 0.02 L of sevoflurane. If the percentage of sevoflurane is decreased to 1 percent, than the mixture is now composed of 0.99 L of oxygen and 0.01 L of sevoflurane. Intermittent positive pressure ventilation may also be warranted. In addition, ensure that no obstruction is present in the airway. In other instances, VPCs are not treated unless the heart rate exceeds 160 beats/min in dogs or if the VPCs are causing a drop in blood pressure. Treatment with lidocaine or procainamide is usually initiated.
Other types of arrhythmias can also occur in anesthetized patients. Ventricular tachycardia occurs when the heart rate exceeds 160 beats/min and the P waves are lost in the QRS complex. Ventricular fibrillation occurs when there is disorganized ventricular depolarization, completely desynchronizing the ventricular contractions. There is no heart beat or pulse, and the ECG has no pattern. This condition will rapidly lead to death. Atrial fibrillation (Figure 2) is an arrhythmia identified on the ECG as tall, narrow QRS complexes with a characteristically irregular rhythm (most commonly at an elevated rate) and no detectable P wave.
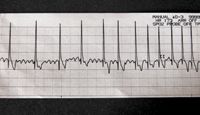
2. Atrial fibrillation. Note the absence of the P wave. It is replaced by the quivering movement between the QRS complexes.
Pulse oximetry
Normal oxygen saturation of hemoglobin values, measured by pulse oximetry (SpO2), range from 95 to 100 percent when a patient is receiving 100 percent oxygen. The pulse rate that is shown next to the SpO2 value should equal the palpated pulse rate and, in most instances, equal the heart rate. The heart and pulse rate may differ if arrhythmias are present. Waveforms should be smooth and consistent. If an irregular waveform is noted, it may indicate an arrhythmia. However SpO2 is not an indicator of how well a patient is ventilating. Many times patients that are hypercapnic (increased end-tidal carbon dioxide values) will have normal SpO2 values. SpO2 values will not increase until the patient is extremely hypercapnic.
Anemic patients may have normal SpO2 values because all available hemoglobin molecules are saturated with oxygen. However, sometimes SpO2 values will be decreased in severely anemic patients. Blood products should be available and given if a patient's PCV is below 21 percent prior to surgery to ensure adequate perfusion of vital organs.
Patients experiencing shock or hypothermia usually have SpO2 values that are abnormally low because of vasoconstriction. If shock is diagnosed, determine the type (cardiogenic, septic, or hypovolemic) and treat accordingly. If the patient is suffering from hypothermia (temperatures less than 97 F), use an external heat source such as convection air warming devices (Bair Hugger—Arizant Healthcare), warmed towels, or rice bags. Exercise caution when using external heating devices because thermal burns may occur. Administering warm fluids is also advisable. Moving the probe to another appendage (e.g., webbing of foot, ear, vulva) may help obtain a more accurate reading in these patients as well as in patients that are undergoing a long anesthetic procedure since the probe itself will cause vasoconstriction if not moved. Wetting or folding the tongue lengthwise in half sometimes aids in increasing the signal.
Patients suffering from hypoxemia (low blood oxygen content) should have their ventilation parameters checked, including their respiration rates and tidal volume (the amount of air inspired or expired during a given breath). Check endotracheal tubes for blood or mucous buildup as well as kinking (a common problem during dental and ophthalmic procedures). Make sure that the fresh gas outlet hose is not kinked, that the oxygen is turned on and hooked up, and that the inspiratory valve is not malfunctioning or warped. Replace warped or malfunctioning valves immediately. If nitrous oxide is being used, it should be turned off until the problem is resolved.
Intermittent positive pressure ventilation can be instituted if the hypoxemia does not resolve. Increasing the overall oxygen percent of the gas mixture by turning down the vaporizer setting may also help resolve the hypoxemia. Finally, check to make sure that the patient isn't suffering from pulmonary edema (due to fluid overloading) or a tension pneumothorax (due to air being left in the chest after thoracotomy).
Noninvasive blood pressure measurement
Noninvasive blood pressure monitoring is most accurate when the mean arterial pressure (MAP) equals 80 to 120 mm Hg or the systolic arterial pressure (SAP) equals 100 to 160 mm Hg. Oscillometric and Doppler methods are considered reliable but may underestimate blood pressure in cats.2 Cuff size should be 40 percent of the circumference of the limb to obtain the most accurate blood pressure reading. A cuff that is too small will overestimate blood pressure, while a cuff that is too large will underestimate blood pressure. The most accurate blood pressure reading is obtained on the forelimb, followed by the hindlimb. Obtaining a blood pressure reading from the tail will give hypertensive results.3 Finally, pulse strength does not equal adequate blood pressure. Hypotensive patients will have easily occluded pulses.
Doppler devices measure SAP. The pulse is made audible by the transducer on the Doppler and aids in detecting arrhythmias. Also, increases in intrathoracic pressure (which will decrease venous return to the heart and, ultimately, blood pressure) can be detected when intermittent positive pressure ventilation is being used since the pulse sound will decrease with each "inspired" breath. The pulse may be difficult to detect if peripheral perfusion is poor.
Oscillometric devices measure MAP, SAP, and diastolic arterial pressure (DAP). Generally, a MAP greater than or equal to 60 mm Hg is needed to provide adequate blood flow to vital organs.3 However, all measurements should be taken into consideration. For example, if MAP is normal, but SAP and DAP are about equal, then the heart may not be performing well (decreased cardiac output). The patient is compensating by increasing peripheral vasoconstriction to maintain adequate blood pressure.4
Capnography
A capnograph assesses ventilation by measuring end-tidal carbon dioxide (ETCO2). ETCO2 approximates arterial concentrations of carbon dioxide and is the amount of carbon dioxide exhaled during each breath. Increases in ETCO2 will occur more rapidly than will decreases in SpO2. Normal values for ETCO2 range between 35 and 45 mm Hg. ETCO2 values greater than 50 mm Hg require manual or mechanical ventilation.
ETCO2 can be analyzed by either side stream or mainstream techniques. Pediatric and adult adaptors are available in both types of monitoring systems (Figure 3). Choosing the correct adaptor is vital for a successful anesthetic experience. Pediatric adaptors help reduce dead space in smaller patients but can increase resistance to flow in larger patients, thus impeding ventilation.

3. An adult adaptor on the left and a pediatric adaptor on the right.
When interpreting ETCO2 data, it is important to analyze the capnograph along with the ETCO2 values since sometimes ETCO2 values alone can be misleading (e.g., tachypneic patients that are hypercapnic). Inspiratory carbon dioxide measurement is available on newer multi-parameter monitors. Inspiratory carbon dioxide should always equal 0 and can aid in troubleshooting stuck or warped one-way valves on an anesthetic machine, alert the anesthetist to depleted soda lime, and aid in identifying clogged or kinked endotracheal tubes. The capnograph can also give important information about the placement of the endotracheal tube or leaks around it and whether the oxygen flow rate for a non-rebreathing anesthesia circuit is appropriate. It can also help you detect apnea, hypoventilation, hyperventilation, or airway obstruction (see the sidebar "Interpreting common capnograph abnormalities").

Interpreting common capnograph abnormalities
Mainstream adaptor windows should be checked regularly for dried mucus or blood, which can prevent the adaptor from reading the ETCO2 correctly (Figure 4). Use warm water on a cotton swab or gauze to gently clean the window. Avoid harsh chemicals. Adaptors can sometimes become dislodged from the cable or become wet during a routine dental prophylaxis. Reattach the adaptor or dry it if it becomes wet, and recommence ETCO2 monitoring. When switching from pediatric to adult adaptors, or vice versa, calibration will be necessary. This is easily done with the calibration device that is usually attached to the ETCO2 cable.

4. An ETCO2 adaptor with dried mucus blocking the window.
Side stream sampling tubes can build up condensation in the line and kink or become clogged. At least three sample lines should be available so that the lines can be alternated among patients and have time to dry. Moisture traps on the monitors can also overfill, causing malfunction of the monitor. Moisture traps should be changed on a regular basis.
Multi-parameter monitors also have the capability to measure and display other values using invasive techniques such as direct blood pressure and central venous pressure. And all monitors come with continual temperature monitoring, which helps prevent patient hypothermia.
Purchasing and maintaining equipment
When purchasing a multi-parameter monitor, the adage that you get what you pay for is definitely true. Paying more upfront will save a practice over the long term. It is advisable to contact large specialty hospitals and veterinary medical teaching hospitals to get advice on what to buy and what to avoid. High-quality monitors should and will last the hospital many years without much service and help you obtain consistent and reliable results. Regular inspection and maintenance of any hospital equipment is important. Cables will need to be replaced from time to time, depending on wear, and all hospitals should carry at least one back-up cable so that dependable monitors are available at all times.
Understanding and interpreting data from a multi-parameter monitor is paramount to a successful anesthetic experience for the technician, the owner, and, most importantly, the patient.
Susan Burns, BS, RVT, VTS (Anesthesia) is a technician at East Bay Veterinary Specialists, in Walnut Creek, Calif. She has a private veterinary anesthetic consulting business and speaks on the topics of anesthesia and pain management.
References
1. Congdon J, Marquez M, Niyom S, et al. Evaluation of the sedative and cardiovascular effects of intramuscular administration of dexmedetomidine with and without concurrent atropine administration in dogs. J Am Vet Med Assoc 2011;239(1):81-89.
2. Acierno M, Seaton D, Mitchell M, et al. Agreement between directly measured blood pressure and pressures obtained with three veterinary-specific oscillometric units in cats. J Am Vet Med Assoc 2010;237(4):402-406.
3. Mazzaferro E, Wagner A. Hypotension during anesthesia in dogs and cats: recognition, causes, and treatment. Compend Contin Educ Pract Vet 8; 2001;728-736.
4. Reuss-Lamky H. Monitoring BP and ETCO2 in anesthetized patients. In Bryant S, ed. Anesthesia for veterinary technicians. 1st ed. Ames, Iowa: Wiley-Blackwell, 2010;112.