Anemia: Its not only about bleeding!
Let's get to the bloody basics of defects in red blood cells, how they can cause anemia and what you (yes, you!) can do about it.
CVC speaker Kenichiro Yagi, MS, RVT, VTS (ECC, SAIM), wants to talk about blood. Specifically, the fact that defects in red blood cells (RBCs) cause the body to destroy them faster than it can produce them, leading to anemia. At a recent CVC Yagi examined issues of anemia–including its causes and how to treat it.
Consider this. Yagi says hemolysis, or the destruction of RBCs, can occur intravascularly where RBCs are destroyed within the bloodstream, or extravascularly, where RBCs are phagocytosed by macrophages in the liver, spleen, bone marrow and lymph nodes.
Intravascular hemolysis causes hemoglobinemia and, when the renal threshold is exceeded, hemoglobinuria, which can cause tubular necrosis and acute renal damage in people-and in some cases, even veterinary patients. In some cases, Yagi says bilirubinemia and bilirubinuria are also seen. Hemolytic anemia is usually regenerative, and additional laboratory signs associated with decreased oxygen-carrying capacity include metabolic acidosis and increased lactate.
Extravascular hemolysis can cause splenic enlargement, Yagi says. Other signs of hemolysis, whether intra- or extravascular, include weakness and pale mucous membranes. Jaundice is noted when the liver's ability to process bilirubin is exceeded. When the oxygen extraction ratio dips below 60% to 70%, clinical signs of decompensation as a result of low hemoglobin concentrations will occur, including weakness, lethargy, tachycardia, tachypnea, impaired mentation or dyspnea.
Let's talk causes
Hemolysis is most commonly caused by acquired defects in RBC membranes that lead to osmotic lysis or phagocytic removal. And Yagi says it's less often a primary or genetic defect.
Can one penny kill an animal? LD50 of zinc is 100 mg/kg. One penny is 2,400 mg/zinc and can kill dogs smaller than 50 pounds.
Heinz bodies: RBC membrane defects due to Heinz body formation may be caused by toxins in food (garlic, propylene glycol, onions), drugs (acetaminophen, vitamin K) and chemicals (zinc, copper). Cats are usually more prone to Heinz body formation-however, due to their increased RBC lifespan, they can show Heinz bodies without anemia. Diabetes mellitus, lymphoma and hyperthyroidism increase the risk of Heinz body anemia in cats. Hypophosphatemia secondary to diabetes mellitus or hepatic lipidosis can increase hemolysis, and phosphate supplementation is recommended if plasma concentrations fall beneath 0.5 mmol/L.
Infections: Bloodborne infections, such as those caused by Babesia canis and Cytauxzoon felis, can cause animals to acquire hemolytic anemia.
Autoimmune: Microscopic examination of blood cells will reveal spherocytes (RBCs that have lost their concave structure) due to phagocytic loss of RBC membranes and gross agglutination (Figure 1). Just remember, immune-mediated hemolytic anemia (IMHA) can occur without agglutination as well.
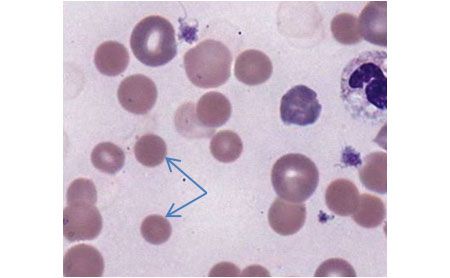
Figure 1: Spherocytes on a blood smear (arrows). (All photos courtesy of Ken Yagi)
Causes of secondary IMHA include neoplasia, drug administration, infection and blood transfusion. Mechanical causes of turbulence in the blood stream, such as heartworm disease, severe cardiac regurgitation, patent ductus arteriosus or hemangiosarcoma may also be at fault. RBCs that have been damaged due to mechanical causes will show fragmented schistocytes (Figure 2) and keratocytes (Figure 3) on blood smears. Neonatal isoerythrolysis, seen in blood type A kittens given colostrum from type B queens, can also cause secondary IMHA.
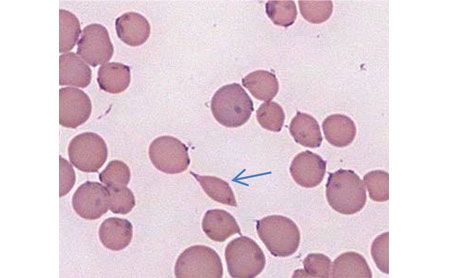
Figure 2: A schistocyte on a blood smear (arrow).
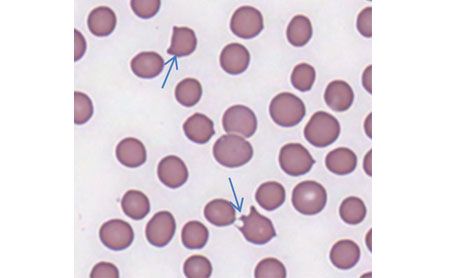
Figure 3: Keratocytes on a blood smear (arrows).
When a secondary cause can't be found, hemolysis is determined to be primary or autoimmune hemolytic anemia.
Genetic: Though rare, genetic defects of RBCs such as elliptocytes, stomatocytes and pyruvate kinase defects, spectrin deficiency and phosphofructokinase defects reduce the lifespan of RBCs.
Time for treatment
Treatment of hemolysis is twofold:
1. Remove the cause of the hemolysis.
2. Support oxygen-carrying capacity with supplemental oxygen or blood products as needed.
Patients with Heinz body anemia must have the source removed (for example, surgical removal of a penny or change in diet). Patients that have been exposed to acetaminophen should be treated with acetylcysteine. Mechanical causes should be addressed, and IMHA is treated with immunosuppressive agents such as glucocorticoids, cyclosporine, mycophenolate, azathioprine or intravenous immunoglobulin.
When the anemia leads to clinical signs associated with hypoxia, supplement oxygen-carrying capacity with packed RBCs to minimize the risk of fluid overload. Check out the links below to find even more on this topic, as well as more great content from Yagi.